Abstract
Introduction: Higher-risk myelodysplastic syndromes (HR-MDS) are rare hematopoietic cancers. While hypomethylating agents (HMAs) are the standard of care, transfusions are important to manage symptoms of anemia and thrombocytopenia. This study aims to better understand the transfusion burden in these patients at baseline and how it is impacted post-HMA initiation, as well as the healthcare resource utilization (HRU) and costs amongst patients with HR-MDS post-HMA initiation, according to baseline transfusion status.
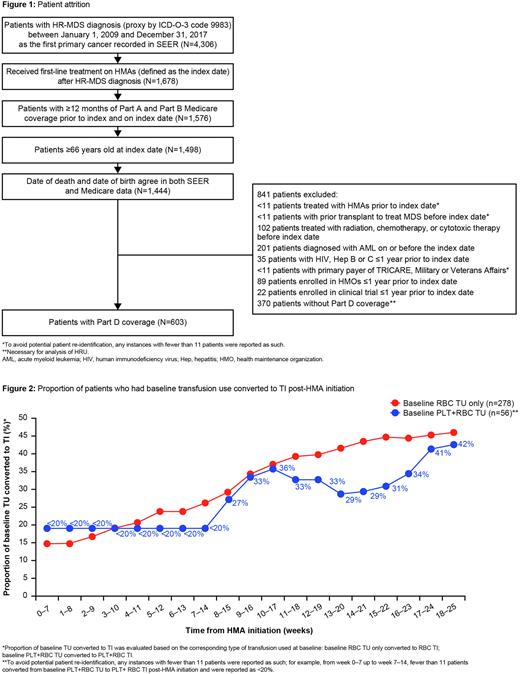
Methods: A retrospective observational study using the Surveillance, Epidemiology, and End Results (SEER)-Medicare linked database. Patients aged ≥66 years, who initiated HMAs after being diagnosed with refractory anemia with excess blasts (a proxy for HR-MDS) between January 1, 2009 and December 31, 2017 were included. Patients were followed up until December 31, 2019 or date of death, whichever occurred earlier. Baseline transfusion status was defined during the 8-week period prior to HMA initiation. Transfusion naïve (TN) patients had no platelet (PLT) or red blood cell (RBC) transfusion episodes. Transfusion users (TU) had ≥1 PLT and/or RBC transfusion episodes. Baseline TU were stratified into PLT TU only, RBC TU only, and PLT+RBC TU. Transfusion independence (TI) was defined as no transfusion episode during an 8-week period. The conversion of baseline TU to TI was evaluated by corresponding transfusion type on a weekly rolling basis post-HMA initiation for 6 months (i.e. week 0-7, week 1-8, through to week 18-25). All-cause HRU and costs (adjusted to 2021 US dollars) post-HMA initiation were evaluated in terms of per-patient-per-month (PPPM) by baseline transfusion status.
Results: In total, 603 patients treated with HMAs met the study criteria (Figure 1). Overall, 42% (254/603) of patients were baseline TN vs 58% (349/603) who were baseline TU (median age: 76 vs 77 years; male: 37% vs 38%; Charlson Comorbidity Index ≥3: 50% vs 64%; median follow-up: 17.0 vs 10.4 months, respectively). Amongst baseline TU, 80% (278/349) were RBC TU only, 16% (56/349) were PLT+RBC TU, and 4% (15/349) were PLT TU only. The median treatment duration of baseline TU receiving HMAs was 6.2 months. By the end of the first 8 weeks post-HMA initiation (week 0-7), 15% of the baseline RBC TU converted to RBC TI, and <20% of baseline PLT+RBC TU converted to PLT+RBC TI. The proportion of baseline RBC TU only who converted to RBC TI post-HMA initiation increased steadily over time; while varying degrees of conversion of baseline PLT+RBC TU to PLT+RBC TI was observed. The conversion of baseline TU to corresponding type of TI stabilized by 17-24 weeks post-HMA initiation: 45% for baseline RBC TU only, and 41% for baseline PLT+RBC TU (Figure 2). Of the baseline PLT TU only cohort, fewer than 11 patients converted to PLT TI at any weekly rolling basis post-HMA initiation. Baseline TN was associated with a lower all-cause HRU PPPM relative to baseline TU: mean (standard deviation [SD]), respectively, was 0.3 [0.5] vs 0.8 [1.4] for inpatient episodes, 0.3 [0.4] vs 0.8 [1.6] for emergency room visits, and 3.3 [2.8] vs 5.9 [15.5] for outpatient visits, p<0.001. Similarly, baseline TN status was associated with a lower total cost of care PPPM compared with baseline TU (mean [SD] of $20,713 [$14,361] vs $36,159 [$99,174], p=0.007). Inpatient cost was the main contributor to the total cost of care (mean [SD] of $7,418 [$9,790] for baseline TN vs $10,722 [$21,823] for baseline TU, p=0.15).
Conclusions: Findings from this study demonstrated the transfusion burden amongst patients with HR-MDS. Nearly 60% of patients with HR-MDS were baseline TU. Although the specific cause of HRU cannot be identified in the database, baseline transfusion use was associated with higher all-cause HRU and total cost of care relative to baseline TN status. The majority (80%) of the baseline TU were RBC TU only. While the conversion from baseline RBC TU only to RBC TI was low (15%) by the end of the first 8 weeks post-HMA initiation, it increased over time, and stabilized at 45% by week 17-24 post-HMA initiation. These findings emphasize that novel treatments are needed for more rapid conversion of baseline TU to TI, and more sustained TI.
Disclosures
Zeidan:Novartis, Cardiff Oncology, Pfizer: Other: Travel Support; Celgene/BMS, AbbVie, Pfizer, Boeringer-Ingelheim, Trovagene, Cardiff Oncology, Incyte, Takeda, Novartis, Aprea, Amgen, Otsuka: Consultancy, Honoraria, Research Funding; Jazz, Agios, Acceleron, Astellas, Daiichi Sankyo, Cardinal Health, Taiho, Seattle Genetics, Beyondspring, Gilead, Kura, Tyme, Janssen, Syndax, Geron, Ionis, Epizyme: Consultancy, Honoraria; Astex, Medimmune, Astrazeneca, ADC Therapeutics: Research Funding; Celgene/BMS, Novartis, Cardiff Oncology, AbbVie: Consultancy, Honoraria, Other: Advisory Board; Celgene/BMS, Novartis, Cardiff Oncology, AbbVie, Pfizer, Boehringer-Ingelheim, Trovagene, Incyte, Takeda, Amgen, Aprea, Astex, Pfizer, Medimmune/AstraZeneca, ADC Therapeutics: Research Funding; Gilead, Kura, Loxo Oncology: Consultancy, Honoraria, Other: Clinical Trial Committee; Celgene/BMS, Novartis, AbbVie, Gilead, Kura, Loxo Oncology, Geron: Other: Clinical Trial Committee; Pfizer, Boehringer-Ingelheim, Trovagene, Incyte, Takeda, Amgen, Aprea, Gilead, Kura, Loxo Oncology, Otsuka, Jazz, Agios, Acceleron, Astellas, Daiichi-Sankyo, Cardinal Health, Taiho, Seattle Genetics, BeyondSpring, Ionis, Epizyme, Janssen, Syndax, Genentec: Consultancy, Honoraria, Other: Advisory Boards. Ng:F. Hoffman-La Roche Ltd.: Current equity holder in publicly-traded company; Genentech: Current Employment. Yellow-Duke:Genentech: Current Employment; Roche, Genentech: Current equity holder in publicly-traded company. Lamarre:Genesis Research: Current Employment. Cheng:AbbVie: Current Employment, Current equity holder in private company, Current holder of stock options in a privately-held company. Ma:Genentech, Inc.: Current Employment, Current equity holder in publicly-traded company.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal